Decoding The Heart's Whispers: Your Guide To ECG Leads
Have you ever wondered how doctors get such a clear picture of your heart's electrical rhythm? It's really quite fascinating, and it all comes down to something called ECG leads. These aren't just simple wires; they are the heart's storytellers, translating tiny electrical signals into a visual language that helps medical professionals understand how well your heart is working. So, you know, getting a good grasp of what these leads do is pretty important for anyone curious about cardiac health or even for those just starting out in medical fields.
The electrocardiogram, often called an ECG or EKG, stands as a very enduring tool in the world of heart care, right alongside the stethoscope. It's actually one of the most efficient ways to check on the heart. This test helps identify a whole range of heart conditions, from heart attacks, which are also known as myocardial infarctions, to issues with the heart's rhythm, like ventricular fibrillation, or even problems with the electrical pathways, such as bundle branch blocks. Basically, the information it provides can be life-saving.
To get accurate results from an ECG, knowing where to put the different leads is absolutely key. This knowledge doesn't just help with reading the results correctly; it also makes sure the information gathered is truly helpful for diagnosis. Without proper placement, you see, the heart's electrical activity might not be captured right, which could lead to missed cues or even wrong conclusions. So, it's pretty clear that understanding these leads is a big deal.
Table of Contents
- What Are ECG Leads, Anyway?
- The Electrode Connection
- Different Views of the Heart
- Understanding Einthoven's Law and the Triangle
- Types of ECG Leads and Their Purpose
- Accurate Placement Matters a Lot
- How Electrical Waves Create ECG Readings
- Interpreting the Signals
- Frequently Asked Questions About ECG Leads
- Bringing It All Together
What Are ECG Leads, Anyway?
The term ‘lead’ in the context of an ECG can be a bit confusing, honestly. When people talk about a "12-lead ECG," it doesn't mean there are 12 physical wires stuck to your body. No, that's not it at all. What it actually means is that these ECGs create 12 different "views" of your heart's electrical goings-on. These specific viewpoints, or perspectives, are what we call ‘leads’. It's like having multiple cameras around an object to see it from all sides, you know, to get the full picture.
These views are derived from a smaller number of physical electrodes. For a standard 12-lead ECG, for example, you typically only need 10 physical electrodes placed on the body. These electrodes then work together, so, to pick up the electrical signals. Each lead gives us information about how positive charges are moving within the heart. This movement is really what tells us a lot about the heart's health and function, actually.
Understanding these leads is quite fundamental because they inform us about the heart's electrical activity from various angles. This helps in localizing where any issues might be. It's like having a map where each lead is a specific point on that map, showing you what's happening in that particular area of the heart. This spatial orientation of the electrical waves is very important for proper diagnosis, basically.
The Electrode Connection
Before we can even talk about leads, we first need to get the electrodes onto the patient’s body. These small, sticky patches are what actually pick up the heart’s electrical signals. They are placed at specific spots to measure and record the electrical activity. You see, proper placement of these electrodes is absolutely vital for getting readings that are accurate and helpful for diagnosis. If they are in the wrong spot, the information you get could be misleading, which is something nobody wants.
The electrical potential of the heart, which is just a fancy way of saying its electrical charge, is registered by these electrodes. They act as sensors, picking up the tiny changes in voltage that happen as the heart muscle contracts and relaxes. It’s pretty amazing how such small signals can tell us so much about a powerful organ like the heart. The way these electrodes are positioned, you know, directly influences the "view" that each lead provides.
So, the electrodes are the physical connection to the body, and the leads are the different perspectives created from those connections. It's a bit like how a photographer might use different lenses or camera angles to capture a subject in various ways. The more precise the electrode placement, the clearer and more reliable the electrical signals will be, and that, arguably, makes all the difference in getting a good ECG reading.
Different Views of the Heart
When we talk about ECGs, you’ll most commonly hear about 3-lead or 12-lead systems. A 3-lead ECG offers a basic overview, often used for continuous monitoring in hospitals, for instance. It gives a general idea of heart rhythm. However, for a more detailed picture, the 12-lead ECG is the gold standard in many settings. It provides a much broader look at the heart’s electrical activity, allowing doctors to spot more subtle issues.
The advantage of using multiple leads is pretty straightforward: each lead provides insights into different areas of the heart. Imagine trying to describe a house if you could only look at it from one window. You’d miss a lot, right? Similarly, a single ECG lead wouldn't give enough information to fully assess the heart's condition. Multiple viewpoints, you know, let us link electrical signals to specific anatomical regions of the heart and even their associated coronary arteries.
This ability to get various viewpoints is why ECGs are so effective for evaluating the heart. They allow for a comprehensive assessment of cardiac health, helping to identify conditions like arrhythmias, which are irregular heartbeats, and myocardial infarctions, or heart attacks. It's really about getting enough information to make an informed decision about someone's heart health, and multiple leads definitely help with that.
Understanding Einthoven's Law and the Triangle
A fundamental concept in ECG interpretation, especially for the limb leads, is Einthoven’s Law. This law, which is pretty neat, describes a specific relationship between three of the standard limb leads: Lead I, Lead II, and Lead III. It basically states that the electrical activity seen in Lead II is equal to the sum of the corresponding activity in Lead I and Lead III. So, it's given as the simple equation: II = I + III. This principle helps confirm the accuracy of readings and provides a framework for understanding how these leads relate to each other.
To give you an example, if you had an ECG where the R wave in Lead I measured 7mm tall and the S wave was 2mm tall, you’d subtract the S from the R, leaving you with 5mm for Lead I. Then, if on the corresponding complex in Lead III, the R wave measured 1mm and the S wave had a negative deflection, you would combine these values. According to Einthoven’s Law, the resulting value for Lead II should match the sum of these two, which is pretty clever, actually. This mathematical relationship is a cornerstone for basic ECG interpretation.
This law is visualized through what’s known as Einthoven’s Triangle. This is an imaginary equilateral triangle formed by the placement of electrodes on the right arm, left arm, and left leg. The heart is considered to be at the center of this triangle. The sides of the triangle represent the three bipolar limb leads (I, II, and III), each measuring the electrical potential difference between two points. It's a really helpful way to picture how these leads are oriented and how they pick up the heart's electrical signals. This geometric representation, you know, makes the whole concept a lot clearer.
Types of ECG Leads and Their Purpose
The various types of ECG leads are designed to give us different "views" of the heart, allowing us to see how positive charges move along different planes. This is incredibly useful for localizing any pathologies, or problems, within the heart. Each type of lead has its own specific placement and provides unique information, which is why we use so many of them. It's not just for fun, you see, it's about getting the most complete picture possible.
Limb Leads
Limb leads are the first set of leads typically discussed, and they are placed on the arms and legs. There are six limb leads in total. Three of these are called bipolar leads: Lead I, Lead II, and Lead III. These measure the electrical difference between two points. Lead I, for instance, looks at the electrical activity between the right arm and the left arm. Lead II looks between the right arm and the left leg, and Lead III looks between the left arm and the left leg. They are really fundamental, in a way, to understanding the heart's overall electrical axis.
The other three limb leads are called augmented unipolar leads: aVR, aVL, and aVF. These leads measure the electrical potential at a single limb relative to a calculated "central terminal" that averages the potential of the other two limbs. So, aVR looks at the heart from the right arm's perspective, aVL from the left arm, and aVF from the left foot. These provide additional angles, you know, to help piece together the heart's electrical story. Together, the six limb leads give us a vertical or frontal plane view of the heart's electrical activity.
Proper placement for these limb leads is pretty straightforward but still very important. The electrodes are typically placed on the fleshy parts of the limbs, avoiding bony prominences. For example, the right arm electrode usually goes on the right wrist or shoulder area, the left arm on the left wrist or shoulder, and the left leg on the left ankle or lower leg. The right leg electrode often serves as a ground. This careful positioning ensures that the signals picked up are clear and accurate, which is, honestly, the whole point.
Precordial (Chest) Leads
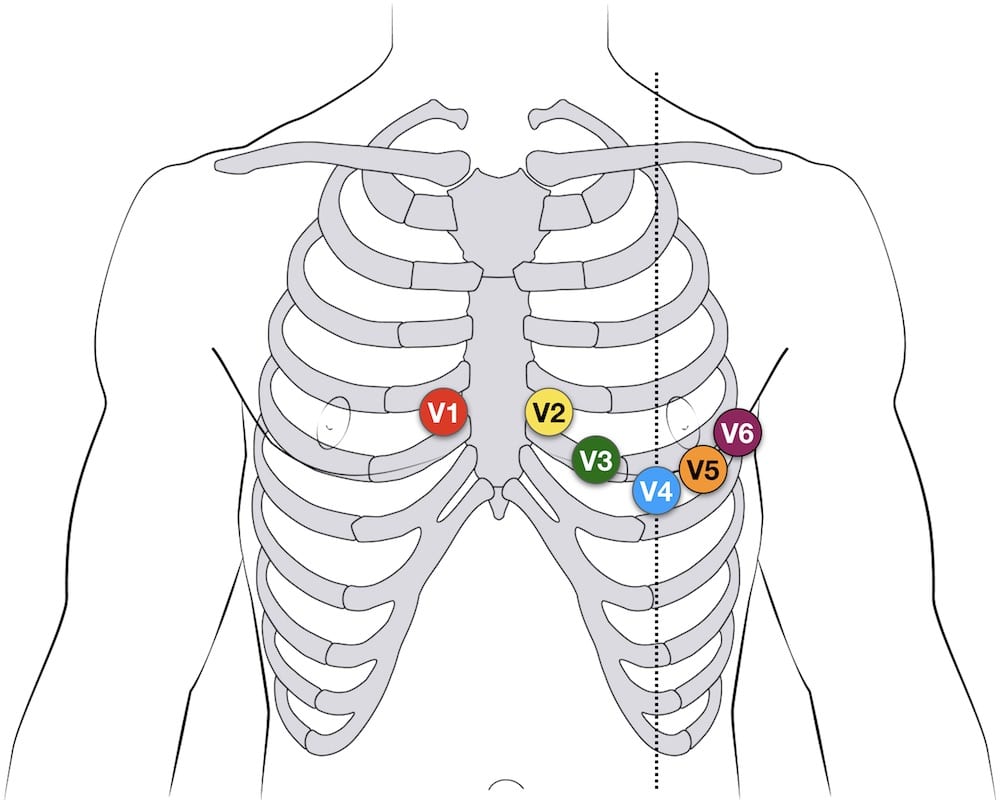
The precordial leads, also known as chest leads, are a set of six unipolar leads (V1 through V6) placed directly on the chest wall. These leads provide a horizontal or transverse plane view of the heart. This means they give us a cross-sectional look at the heart's electrical activity, which is very different from the limb leads. Each precordial lead looks at a specific part of the heart, offering detailed information about the ventricles, for instance.
The placement of these leads is quite precise and follows anatomical landmarks. V1 is placed in the fourth intercostal space (the space between the 4th and 5th ribs) to the right of the sternum. V2 is placed in the same intercostal space but to the left of the sternum. V3 goes halfway between V2 and V4. V4 is placed in the fifth intercostal space in the midclavicular line (under the middle of the collarbone). V5 is in the same horizontal line as V4, in the anterior axillary line (front of the armpit). And V6 is also in the same horizontal line as V4 and V5, but in the midaxillary line (middle of the armpit). Getting these spots just right, you know, is absolutely crucial for accurate readings.
These chest leads are particularly valuable for diagnosing conditions like myocardial infarctions because they can pinpoint exactly which part of the heart muscle might be experiencing damage. For example, changes in V1 and V2 might suggest an issue with the septum, while changes in V5 and V6 could point to the lateral wall. So, they provide very localized information that the limb leads might not capture as clearly, which is why they are so important.
Extended Views: Posterior and Right-Sided Leads
While the standard 12-lead ECG is very comprehensive, sometimes a doctor needs even more specific information. This is where extended views, like posterior and right-sided leads, come into play. A 15-lead ECG, for example, typically includes the standard 12 leads plus three additional ones: RV4, V8, and V9. These extra leads are used when there's a suspicion of an issue in an area of the heart not fully covered by the standard leads. It’s pretty clever, really, how they adapt the test for more detailed insights.
RV4 is a right-sided precordial lead, placed on the right side of the chest in the same position as V4 would be on the left. This lead is especially helpful for detecting right ventricular heart attacks, which are less common but very serious. V8 and V9 are posterior leads, placed on the back to visualize the posterior wall of the left ventricle. V8 is placed at the same horizontal level as V6, but on the posterior axillary line (back of the armpit), and V9 is also at the same level, but next to the spine. These are often used when there’s a suspicion of a posterior myocardial infarction, which might not show up clearly on the standard 12 leads. So, these extra views, you know, can make a big difference in diagnosis.
The ability to add these specialized leads shows how versatile the ECG system can be. It allows medical professionals to tailor the assessment based on the patient's symptoms and what they suspect might be happening. This adaptability means they can get the most accurate picture possible of the heart's electrical activity, even in tricky situations. It’s a bit like zooming in on a specific part of a map when you need more detail, which is very useful, as a matter of fact.
Accurate Placement Matters a Lot
We’ve touched on it already, but it really can’t be stressed enough: proper placement of electrodes is absolutely essential for accurate ECG readings and, by extension, for an effective diagnosis. Incorrect placement can lead to what are called "artifact" or misleading readings, which can cause confusion and potentially delay proper treatment. It's like trying to listen to a conversation through a wall; you might hear something, but it won't be clear. You know, getting it right the first time saves a lot of trouble.
Understanding the correct placement techniques can significantly enhance the quality of the ECG results. This includes knowing where to place limb and chest leads accurately and consistently, every single time. There are guides, and even videos, that show the ultimate way to do this. For instance, using consistent anatomical landmarks helps ensure that the leads are always in the right spot, regardless of who is performing the test. This consistency, in a way, builds reliability into the process.
When you place the electrodes just right, the ECG uses its multiple viewpoints to truly link electrical signals to specific anatomical regions of the heart. This connection is vital for understanding how electrical waves affect the readings, whether they are depolarization waves (showing contraction), repolarization waves (showing relaxation), or even biphasic waves (showing activity moving in two directions). Without accurate placement, these crucial details might be distorted or completely missed, which is a big deal, frankly.
How Electrical Waves Create ECG Readings
The heart generates electrical activity through a process of depolarization and repolarization of its muscle cells. Depolarization is essentially the electrical activation that leads to muscle contraction, while repolarization is the electrical recovery that allows the muscle to relax. These waves of electrical activity spread throughout the heart in a very organized fashion. The ECG machine, you see, picks up these tiny electrical currents as they travel, turning them into the squiggly lines you see on the ECG paper.
When an electrical wave moves towards a positive electrode, it creates an upward deflection on the ECG tracing. If it moves away from a positive electrode, it creates a downward deflection. And if the wave moves perpendicularly to the electrode, it might create a biphasic wave, meaning it goes both up and down. This relationship between the direction of electrical flow and the deflection on the paper is fundamental to interpreting what the heart is doing. It’s pretty much how the machine translates the heart’s language into a visual format, actually.
Understanding these basic components of the ECG, like the lead system used to record the tracings, is really important. The ECG waves and intervals, along with their spatial orientation, tell a detailed story about the heart’s electrical health. For example, the P wave represents atrial depolarization, the QRS complex represents ventricular depolarization, and the T wave represents ventricular repolarization. Each part of the tracing corresponds to a specific electrical event in the heart, and knowing what each part means is very helpful for diagnosis, obviously.
Interpreting the Signals
Once the ECG tracings are recorded, the real work of interpretation begins. This involves looking at the patterns of the waves, the intervals between them, and how they appear across all the different leads. Because each lead offers a unique view of the heart, combining the information from all leads allows for a comprehensive assessment. This skill of ECG interpretation is a vital diagnostic skill in any medical setting, honestly, because it’s so widely used.
For example, if a doctor suspects a heart attack, they would look for specific changes in certain leads. ST-segment elevation in particular leads can point to a myocardial infarction and even tell them which coronary artery might be blocked. Similarly, abnormal rhythms, or arrhythmias, can be identified by looking at the regularity and shape of the waves across the leads. It’s like putting together pieces of a puzzle, where each lead provides a crucial piece of information. This process, you know, helps identify a wide range of heart issues.
The medical uses for this information are varied and often need to be combined with knowledge of the structure of the heart and physical examination signs to be fully interpreted. An ECG alone provides electrical data, but when combined with a patient's symptoms, medical history, and other test results, it becomes an incredibly powerful diagnostic tool. So, a basic knowledge of the ECG will definitely enhance anyone's overall understanding of cardiology, which is a pretty good thing to have.
Frequently Asked Questions About ECG Leads
What is the difference between an electrode and a lead in ECG?
Well, an electrode is the actual sticky patch placed on the patient's skin that picks up the heart's electrical signals. A lead, on the other hand, is a specific "view" or perspective of the heart's electrical activity that is created by combining the signals from two or more electrodes, or from one electrode and a calculated reference point. So, you know, you might have 10 electrodes on someone, but they generate 12 different leads or views.
Why do we use multiple leads for an ECG?
We use multiple leads because the heart is a three-dimensional organ, and its electrical activity spreads in many directions. Each lead offers a unique viewpoint, allowing doctors to see different areas of the heart from various angles. This helps in pinpointing the exact location of any electrical problems or damage, which is pretty important for accurate diagnosis. It's like having many cameras around a building to see all its sides, you see.
Can incorrect ECG lead placement affect the diagnosis?
Absolutely, yes. Incorrect lead placement can significantly distort the electrical signals picked up by the ECG machine, leading to inaccurate readings. This can result in misinterpreting the heart's condition, potentially causing a wrong diagnosis or delaying appropriate treatment. So, it's pretty crucial to place them correctly every time, honestly, to get reliable information.
Bringing It All Together
Understanding ECG leads is a foundational step for anyone interested in cardiac health, whether you’re a student, a healthcare professional, or just curious. These leads, derived from carefully placed electrodes, provide invaluable insights into the heart's electrical activity. From the basic limb leads that give a frontal view to the detailed precordial leads that offer a cross-sectional look, and even the specialized posterior and right-sided leads, each one contributes to a complete picture of the heart's well-being. Knowing where to place them accurately and how to interpret their signals is what makes the ECG such a powerful diagnostic tool. It really helps to visualize charge movement along different planes and localize pathologies, you know, allowing for precise identification of issues like myocardial infarction, ventricular fibrillation, or bundle branch blocks. To learn more about ECG interpretation on our site, and for more specific details about lead systems, you can also check out basic components of the ECG and the lead system.
ECG Lead positioning • LITFL • ECG Library Basics

ECGs: Colour-coding for initial training - Resuscitation

Alila Medical Media | 12-lead ECG | Medical illustration